- Home
- About Us
- Research
- Research Areas
- Agriculture
- Air Pollution
- Climate Change
- Economy
- Education
- Environmental Law & Justice
- Energy & Electricity
- Federalism
- Governance, Accountability & Public Finance
- Health & Nutrition
- Indian Politics
- International Relations & Security
- Jobs
- Land Rights
- Sanitation
- Social Justice
- State Capacity
- Technology
- Urbanisation
- Water
- Miscellaneous
- Research Initiatives
- Accountability Initiative
- Governance & Public Policy Initiative
- India Infrastructures & Ecologies Program
- Initiative on Cities, Economy & Society
- Initiative on Climate, Energy & Environment
- Land Rights Initiative
- Scaling City Institutions for India Initiative (SCI-FI)
- State Capacity Initiative
- The Jobs Initiative
- The Politics Initiative
- The Technology & Society Initiative
- TREADS: Transboundary Rivers, Ecologies & Development Studies
- Research Areas
- Publications
- People
- Events
Highlight>
Unpacking India’s Second COVID-19 Wave and Vaccination Strategy
April 5, 2021

India’s vaccination drive began in January 2021. The recent rise in daily COVID-19 cases and deaths however, has been worrying. What led to the second surge in the country? How has the vaccination drive fared so far? Is India’s vaccination strategy the correct one? As certain states account for majority of the cases, how should the government alter its approach to contain the spread of the virus? Partha Mukhopadhyay, Senior Fellow at CPR, who has been closely tracking the pandemic, sheds light in this interview.
What according to you are the reasons for India’s second surge? A few months ago, we witnessed a steady decline in new cases. What has happened?
The short answer is: we don’t know. The other answer is: it had to happen. The surprise in India was that cases were going down steadily since mid-September, even as behaviour was becoming less and less CoVID-appropriate. It had to happen sometime and it happened in early to mid-February.
If the nature of CoVID infections is heterogeneous, i.e., (i) a few people mix with a lot of people and most people mix with few people and (ii) a few infected people infect a lot of people and lot of infected people do not infect others (or very few), then, it is the case that these kinds of localised spurts in infections can happen as part of the evolution of the pandemic. This is one of the results that we showed in our paper. So, from that perspective, this is not unusual.
There can be other, more deterministic, explanations, such as a variant, infective strain such as the B.1.1.7 variant that appears to dominate samples from Punjab or super-spreader events like election gatherings. Not enough information is being released about variants and genomic sequencing to answer this question, but it is odd that the Maharashtra surge started away from the major metros of the Golden Triangle (Nashik, Pune, Mumbai) in the smaller towns of Vidarbha, which is less likely to have imported variants. These areas were holding Gram Panchayat elections and celebrations took place in late January, but this also sounds a little over-determined since a lot of gatherings have been taking place around the country. A number of cases in Maharashtra were also reported from school hostels, after re-opening.
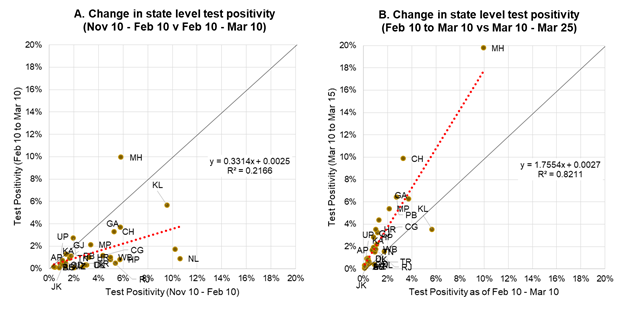
There is no particular evidence that testing in some states were low relative to other states, though it did decline for all states. Nor are there striking differences in mobility across states. But, wherever it started, it is now clear that the spread is much wider, as seen in Figure 1. In panel A, it is seen that the positivity (people testing positive as a share of people tested) in February 10 – March 10 of 2021 is much less than that over the period November 10, 2020 – February 10, 2021, except for Maharashtra, which had already started rising by this time. However, when we look at March 10-25, compared to the Feb – March period, in panel B, we see a striking increase in positivity in many states, indicating the spread of the second surge.
It is perhaps useful here to address the issue of sero-positivity surveys and herd immunity. Some commentators attributed the decline that occurred over September to January, to growing herd immunity, pointing to the high level of sero-positivity found in many surveys. However, these surveys seem to be at odds with the current experience, for example, one of the worst hit cities at the moment is Pune, which also had some of the highest sero-positivity numbers reported. It is the same for Bangalore and, also to some extent for Mumbai. It is possible that the current cases are concentrated in particular social classes and age-groups, while the sero-positivity were in other social classes, e.g., slum residents, but this is not something we know without more information.
Even if this sero-positivity hypothesis is accurate, an unexplained part of the hypothesis was the large number of unreported infections – indicating that these were most likely asymptomatic or very mildly symptomatic, also explaining why there was such limited reporting and relatively little pressure on hospitals. In this surge too, a very high proportion of asymptomatic cases is being reported, well over 80% in Mumbai. There has been no explanation for why Indian cases should be so asymptomatic. It is not that infected persons are much younger, though the share of 50+ is about 7% lower.
Another pattern that seems to be repeated from the early days of the pandemic is that a large number of the deaths, while fewer, are happening relatively soon after coming to hospital, implying that they are reporting late or the progression of the disease is suddenly taking a very bad turn for the worse.
India started its vaccination drive in January 2021. How do you think it has fared so far?
We took our time. We first started vaccinating healthcare workers (HCW) in mid-January, then added frontline workers (FLW) in early February and did not open up to the broader population until March. This may have allowed our core vaccination application – CoWIN – to stabilise and be tested on HCWs and FLWs, so as to iron out any glitches before it was rolled out to the general population. We also expanded the range of places that were allowed to vaccinate, including private hospitals and clinics, for a relatively small fee.
On the positive side, apart from a few starting glitches, we seem to not have had the kind of chaos seen in the United States in terms of arranging appointments for vaccination (people who were unable to engage with the web or the app were able to walk in to vaccination centres where they were assisted to enrol and get vaccinated). On the negative side, we seem to be vaccinating below capacity (actual vaccinations well below peak vaccinations, no vaccinations on Sunday, etc.) and possibly focusing more on the urban and peri-urban areas.
Also, we are only using two vaccines, Covishield and Covaxin (about 10% of the vaccines administered). We may have been able to expand capacity if we had allowed import of other vaccines like Pfizer-BioNTech and Moderna, which may not have been usable in many areas but which could have expanded supply in larger cities and private hospitals. We could have also imported other, less expensive, vaccines proposed to be manufactured in India, such as Sputnik V, which could be administered more widely (though with trained vaccination personnel because of the need to reconstitute, like Pfizer-BioNTech). But, we may have been prevented from doing so due to supply limitations.
The final concern that I have is that there is almost no outreach, no exhortation to get vaccinated, none of the saturation do gaz ki doori, mask hai zaroori that we saw for non-pharmaceutical interventions during the pandemic. There is also no concerned effort to bring vaccination centres closer to the people, though this is happening at a local level in some places, e.g., vaccination camps in community centres, apartment complexes, etc.
We were fortunate to begin the vaccination drive at a time when CoVID cases were dipping. On 1st April, we opened up the drive to all individuals above 45, amidst a second surge. Do you think we should have inoculated as many people as possible earlier, while cases were low, to avoid this situation? Is this a missed opportunity of sorts?
Yes, we could have vaccinated over 100 million people by now, if we had been able to advance the vaccination process by a month, starting the general population in February instead of March, if the app and web platform was operational and the supplies in place. Broadly speaking our most vulnerable are the persons over 60 who account for over half our deaths and those between 45 and 59 who account for another one-third. Among these, the most exposed are those living in urban areas. There are about 40 million people in urban areas above 60 years of age and another 60 million between 45 and 59. So, by now, we could have given all of these people at least one dose of the vaccine, if they had chosen to come forward to be vaccinated.
Since we do not know the rural / urban mix of people vaccinated (even roughly, estimated, for example, by the location of the vaccination centre), we cannot estimate how many people in the target population chose to get vaccinated and how many did not, because of vaccine hesitancy (they do not want to be vaccinated) or vaccine inaccessibility (they would like to be vaccinated but the centre is inaccessible). This is a major shortcoming.
Already, from the data on both the continuing uptake of first doses among HCW and FLW, which should have been completed by February and the share of eligible HCW and FLW who have come back for their second dose, we can see that a significant minority may not be enthusiastic about vaccination.
India’s vaccination strategy has so far been to vaccinate the vulnerable age groups. However given that we see increased mobility (to workplaces, socialising etc.) in younger age groups, would it be fair to assume that they act as super spreaders? In such a scenario, shouldn’t the vaccination strategy target this age group to avoid the spread of the infection between them and from them to older, more vulnerable groups?
Actually, the assumption that younger people infect other people more does not have any empirical support – it is not that it is false, just that there is no evidence for it either way. Indonesia is trying out such a strategy of vaccinating the younger population first (including allowing the private sector to import vaccines and vaccinate its workers), but there are two critical differences to be noted, of vulnerability and feasibility.
As noted earlier, about 85% of the deaths are of people more than 45 years old. This is therefore, the more vulnerable population (in advanced countries, the share of deaths in the 45-59 age group is much lower; less than 5% in Europe, compared to more than 30% in India).
The age group of 45 to 59 comprise 14% of the urban population and that of 60+ comprise another 9%, whereas the 18 to 44 age group makes up 46% of the population, i.e., more five times the number of 60+ people. So, starting with this group is much more feasible.
The vaccination drive has been fairly centralised, with the government exercising strict control. Given certain states like Maharashtra account for the majority of the cases in the country, do you think different states need a different vaccination strategy?
States should definitely have discretion as to where they locate the vaccination centres, etc. and it is my understanding that they do have that flexibility. However, it is more difficult to start vaccinating certain groups in certain locations, earlier, e.g., 30 year olds in Maharashtra compared to other states. It should definitely be possible to do so, in a consultative manner with other states indicating that stopping the surge in Maharashtra is to the benefit of all states, but it is not clear whether that degree of trust and maturity in the federal system has been nurtured by the Union government, and I am not pointing just to this government.
If we had this level of trust and co-operation, we could have definitely prioritised one geography over another. There is some disagreement over which geography should be prioritised, whether it should be the one experiencing a surge, that I would advocate or the one that is vulnerable but not yet infected, e.g., Bihar, but that is a different debate.
This would also help us in deciding when we should expand deeper into rural areas, beyond the urban and urban periphery. Implementing a two-dose vaccination programme in such areas is administratively complex, especially since people are difficult to reach for their second dose, due to shared phones, etc. In such a situation, it may be better to wait for a single-dose vaccine like the Janssen (Johnson and Johnson) vaccine, which will also be manufactured in India, especially since much of rural India has not been touched by the pandemic (though it can be argued that it leaves them more vulnerable).

